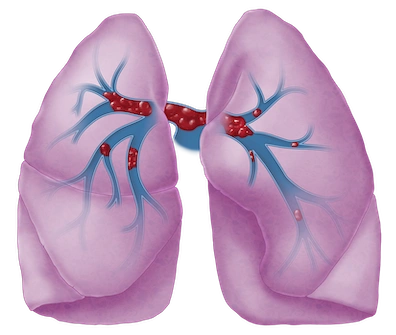
Pulmonary Embolism
Pulmonary embolism (PE) is a potentially life-threatening condition in which blood flow to the lungs is blocked by clot. PE, a type of venous thromboembolism, is usually caused by deep vein thrombosis, a blood clot that partially or completely blocks blood flow through a vein deep in the body, particularly the lower leg, thigh, or pelvis.
More About This Condition
PE occurs when blood clot breaks loose from a deep vein in the body, travels through the bloodstream, and lodges in an artery in the lungs. If left untreated, PE can cause heart attack, shock, stroke, or death. PE can also develop directly in the small blood vessels of the lungs, even if there are no clots in the arms or legs.
IMPORTANT NOTE: This overview is provided for informational purposes only and should not be used as a substitute for talking with your doctor. Be sure to talk with your doctor for a complete discussion of this condition as well as the benefits and risks of any treatment options.
Symptoms of PE can vary depending on the size of the blood clot and where it is located. Some people may not have any symptoms, while others may experience sudden, severe symptoms. Common signs and symptoms of PE include:
- Chest pain or discomfort, which may worsen with deep breathing, coughing, or exertion
- Shortness of breath, which may occur suddenly or gradually
- Rapid or irregular heartbeat
- Coughing up blood
- Sweating
- Dizziness or lightheadedness
Diagnosis
Your doctor may:
- Ask you or a family member about your risk factors, such as high blood pressure, smoking, heart disease, and a personal or family history of blood clots.
- Ask about your signs and symptoms and when they began.
- Conduct a physical examination.
Your doctor may order one or more of the following tests:
- Echocardiography (echo) uses sound waves to create moving pictures of your heart. The pictures show the size and shape of your heart and how well your heart is pumping blood.
- Blood tests measure substances in the blood that may indicate a blood clot. D-dimer tests measure a substance in the blood that is released when a clot breaks up. Troponin is a lab test that measures a protein found in heart muscle, which is released into the blood stream when damage to the heart muscle occurs. A PE can cause damage to the heart, which is why your doctor will order this test.
- Ventilation perfusion (V/Q) scan measures air flow (ventilation) and blood flow (perfusion) in the lungs. If your lungs do not get the right amount of air or blood, you may have PE.
Treatment
Treatment for this condition must always be discussed with your doctor for a full discussion of options, risks, benefits, and other information.
Anticoagulants or blood thinners keep blood clots from getting larger and stop new clots from forming.
Thrombolytics (commonly referred to as “clot busters”) work by dissolving the clot.
Endovascular intervention is another option. Treatment consists of either an injection of a clot-busting drug or mechanical thrombectomy, a minimally invasive procedure that physically removes clot from blocked arteries. The two can be used in combination.
Now, physicians can use computer-aided thrombectomy, which is designed to address blood loss concerns for efficient clot removal across multiple disease states including clots in the lungs.
